 A strong healthcare data protection program goes beyond compliance; here are some pointers for safeguarding healthcare data against today's threats.
A strong healthcare data protection program goes beyond compliance; here are some pointers for safeguarding healthcare data against today's threats.
Data security in the healthcare industry is a difficult task. Healthcare providers and their business associates must strike a balance between protecting patient privacy and providing high-quality patient care while adhering to HIPAA and other regulations, such as the EU's General Data Protection Regulation (GDPR). Because protected health information (PHI) is among an individual's most sensitive (and valuable) private data, the guidelines for healthcare providers and other organizations that handle, use, or transmit patient information include stringent data protection requirements that can result in hefty penalties and fines if not met.
Rather than mandating the use of specific technologies, HIPAA requires covered entities to ensure that patient information is secure, accessible only to authorized individuals, and used only for authorized purposes, but it is up to each covered entity to determine what security measures to employ to achieve these objectives.
As regulatory requirements for healthcare data protection increase, healthcare organizations that take a proactive approach to implementing best practices for healthcare security are best equipped for continued compliance and are less likely to suffer costly data breaches. In this guide, we'll go over 10 data protection best practices for healthcare organizations, including:
- Educating Healthcare Staff
- Restricting Access to Data and Applications
- Implementing Data Usage Controls
- Logging and Monitoring Use
- Encrypting Data
- Securing Mobile Devices
- Mitigating Connected Device Risks
- Conducting Regular Risk Assessments
- Utilizing Off-Site Data Backup
- Carefully Evaluating the Compliance of Business Associates
Let's look at the HIPAA Privacy and Security Rules and how these ten best practices can assist healthcare organizations in maintaining compliance while protecting sensitive health information.
HIPAA Privacy and Security Rules
HIPAA regulations have the greatest impact on healthcare providers in the United States, but other regulations, such as the upcoming GDPR, will have an impact on global operations. It is the responsibility of healthcare providers and business associates to stay up to date on the latest requirements and to select vendors and business associates who are also in compliance with these regulations. HIPAA includes two key components for the protection of healthcare data:
- The HIPAA Security Rule - focuses on ensuring the security of electronic personal health information created, used, received, and maintained by HIPAA-covered organizations. The Security Rule establishes guidelines and standards for the administrative, physical, and technical management of personal health information.
- The HIPAA Privacy Rule - Requires safeguards to protect the privacy of personal health information, such as medical records, insurance information, and other sensitive information. Without prior patient authorization, the Privacy Rule restricts what information may be used (and in what manner) and disclosed to third parties.
The HIPAA Privacy Rule is primarily concerned with operational situations, prohibiting providers and their business associates from using a patient's PHI in ways that were not previously agreed upon by the patient and limiting the information that can be shared with other entities without prior authorization. The HIPAA Security Rule is more concerned with the technical aspects of protecting personal health information, and it establishes standards and regulations for how health information should be safeguarded to ensure the integrity and confidentiality of healthcare data.
The increased use of electronic health records contributes to increased healthcare risk and data breaches.
Healthcare organizations and business associates must implement robust security measures to protect patient data from an increasing number and variety of threats in order to adequately protect data from cybercriminals. Wireless network vulnerabilities, for example, provide an easy entry point for hackers, even though these networks are critical to healthcare organizations, making it easier to access patient information and optimize care delivery.
How to Protect Healthcare Data
These healthcare cybersecurity best practices aim to keep up with the evolving threat landscape by addressing threats to privacy and data protection on endpoints and in the cloud, as well as protecting data while it's in transit, at rest, and in use. This necessitates a multifaceted, sophisticated security strategy.
1. Educate Healthcare Staffs
Human error remains one of the most serious threats to security in all industries, but especially in healthcare. Human error or negligence can have disastrous and costly consequences for healthcare organizations. Security awareness training provides healthcare employees with the knowledge they need to make wise decisions and exercise appropriate caution when handling patient data.
2. Restrict access to data and Applications
Implementing access controls improves healthcare data security by limiting access to patient information and specific applications to only those users who need it to do their jobs. User authentication is required for access restrictions, ensuring that only authorized users have access to protected data. Multi-factor authentication is a recommended approach, which requires users to validate that they are indeed the person authorized to access certain data and applications by using two or more validation methods, such as:
- Information known only to the user, such as a password or PIN number.
- Something that only the authorized user would possess, such as a card or key
- Something unique to the authorized user, such as biometrics (facial recognition, fingerprints, eye scanning)
3. Implement Data Usage Controls
Protective data controls go beyond the benefits of access controls and monitoring to ensure that potentially harmful or malicious data activity is identified and/or blocked in real time. Data controls can be used by healthcare organizations to prevent specific actions involving sensitive data, such as web uploads, unauthorized email sends, copying to external drives, or printing. Data discovery and classification play an important supporting role in this process by ensuring that sensitive data is identified and tagged appropriately.
4. Log and Monitor Use
Logging all access and usage data is also critical, allowing providers and business partners to track which users access what information, applications, and other resources, when, and from which devices and locations. These logs are useful for auditing purposes, assisting organizations in identifying areas of concern and strengthening protective measures as needed. When an incident occurs, an audit trial may allow organizations to identify specific entry points, determine the cause, and assess damages.
5. Encrypt Data at Rest and in Transit
Encryption is one of the most effective methods of data protection for healthcare organizations. Healthcare providers and business associates make it more difficult (ideally impossible) for attackers to decipher patient information even if they gain access to the data by encrypting it in transit and at rest. HIPAA makes recommendations but does not require healthcare organizations to implement data encryption measures; rather, the rule leaves it up to healthcare providers and business associates to determine which encryption methods and other measures are necessary or appropriate given the organization's workflow and other needs.
6. Secure Mobile Devices
Healthcare providers and covered entities are increasingly relying on mobile devices to conduct business, whether it's a physician using a smartphone to access information to help them treat a patient or an administrative worker processing insurance claim. Mobile device security requires a plethora of security measures, including:
- Managing all devices, settings, and configurations
- Enforcing the use of strong passwords
- Enabling the ability to remotely wipe and lock lost or stolen devices
- Encrypting application data
- Monitoring email accounts and attachments to prevent malware infections or unauthorized data exfiltration
- Educating users on mobile device security best practices
- Implementing guidelines or whitelisting policies to ensure that only applications meeting pre-defined criteria or having been pre-vetted can be installed
- Requiring users to keep their devices updated with the latest operating system and application updates
Requiring the installation of mobile security software, such as mobile device management solutions
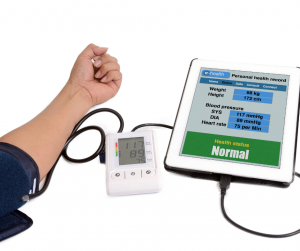
7. Mitigate Connected Device Risks
You probably think of smartphones and tablets when you think of mobile devices. However, with the rise of the Internet of Things (IoT), connected devices are taking on a variety of shapes and sizes. Everything from medical devices like blood pressure monitors to cameras used to monitor physical security on the premises may be network-connected in the healthcare industry. To maintain adequate connected device security, follow these steps:
- Maintain IoT devices on their own separate network
- Continuously monitor IoT device networks to identify sudden changes in activity levels that may indicate a breach
- Disable non-essential services on devices before using them, or remove non-essential services entirely before use
- Use strong, multi-factor authentication whenever possible
Keep all connected devices up to date to ensure that all available patches are implemented
8. Conduct Regular Risks Assessment
While an audit trail aids in determining the cause and other important details of an incident after it has occurred, proactive prevention is equally important. Regular risk assessments can identify vulnerabilities or weak points in a healthcare organization's security, deficiencies in employee education, inadequacies in vendor and business associate security posture, and other areas of concern. By evaluating risk across a healthcare organization on a regular basis in order to proactively identify and mitigate potential risks, healthcare providers and their business associates can better avoid costly data breaches and the many other negative consequences of a data breach, ranging from reputational damage to regulatory penalties.
9. Back up Data to secure, offsite location
Cyberattacks can expose sensitive patient information, but they can also jeopardize data integrity or availability; ransomware is one example of the impact these incidents can have. Even a natural disaster affecting a healthcare organization's data center can be disastrous if data is not properly backed up. That is why frequent offsite data backups are advised, along with strict controls for data encryption, access, and other best practices to ensure the security of data backups. Offsite data backups are also an important part of disaster recovery.
10. Carefully evaluate the security and compliance posture of Business Associates
Because healthcare information is increasingly being transmitted between providers and covered entities for the purposes of facilitating payments and delivering care, one of the most important security measures healthcare organizations can take is a careful evaluation of all potential business associates. The HIPAA Omnibus Rule strengthened previous guidelines and clarified business associate definitions, providing better guidance on the relationships for which contracts are required. These clarifications and changes are summarized in the HIPAA Survival Guide, which includes:
- The conduit exception applies to organizations that transmit personal health information but do not maintain or store it. Organizations that merely transmit data are not business associates, whereas those that maintain and store PHI are.
- When third-party applications and services, such as Google Apps, are used to maintain PHI, they are considered business associates. In such cases, the third-party service would be considered a business associate, necessitating the use of a contract. According to the HIPAA Survival Guide, as more organizations use the cloud, they should be aware of all instances that would make a vendor a business associate, as well as the likelihood of those vendors entering the required contract.
- Subcontractors who create or maintain PHI must follow compliance regulations. This change alone has a significant knock-on effect and should be taken seriously by all healthcare organizations.
- All covered entities must obtain "satisfactory assurances" that PHI will be adequately protected from all vendors, partners, subcontractors, and the like. PHI is subject to liability wherever it goes.
- Some exceptions exist. According to the HIPAA Survival Guide, "in general, a person or entity is a Business Associate only when the person or entity is performing a function or activity regulated by the HIPAA Rules on behalf of a Covered Entity, such as payment or healthcare operations; thus, a researcher is NOT automatically a Business Associate of a Covered Entity, despite the fact that the researcher may be using the Covered Entity's Protected Health Information."
As the preceding clarifications demonstrate, the privacy and security requirements for HIPAA compliance are dependent not only on the activities of a healthcare organization, but also on any ancillary organizations with whom it does business and third-party services with which it works. In other words, one organization's compliance is heavily reliant on its ability to select and collaborate with vendors who employ similarly stringent healthcare data protection measures. Furthermore, healthcare organizations that take data security seriously should understand that, while HIPAA and other regulatory compliance initiatives are a good place to start when developing a data protection program and avoiding costly penalties, efforts should go beyond compliance to ensure that sensitive data is protected against today's threats.



